TPS Commissioning and Quality Assurance
Selected Readings
AAPM MPPG 5 provides the minimum acceptable standards for commissioning and quality assurance of megavoltage photon and electron treatment planning dose calculation software.
AAPM TG-53: Quality Assurance for Clinical Radiotherapy Treatment Planning (External Link)
AAPM TG-53 reports on quality assurance for treatment planning process as well as QA and commissioning of the treatment planning system (TPS).
AAPM TG-106: Accelerator Beam Data Commissioning Equipment and Procedures (External Link)
AAPM TG-106 provides guidance both on accelerator commissioning as well as best practices and minimal required data for TPS commissioning.
AAPM TG-119: IMRT Commissioning (External Link)
AAPM TG-119 provides confidence limits and baseline performance expectations for IMRT based on a multi-institutional comparison of IMRT planning and dosimetry.
AAPM TG-218: Tolerance Limits and Methodologies for IMRT Measurement-Based Quality Assurance (External Link)
AAPM TG-218 analyses the use of various measurement schemas, DTA and gamma-index, to assess agreement between TPS computed dose and delivered dose.
Key Point: Acceptance Testing vs Commissioning
Acceptance testing is performed with the vendor and physicists to assure that hardware and software meet certain predefined expectations.
Commissioning takes place after acceptance of the machine and involves significantly more detailed characterization of the performance of a specific machine and treatment planning system.
Basic Aspects of TPS Commissioning (AAPM TG-53)
AAPM TG-53 provides high level guidance on what aspects of a TPS system must be commissioned. Generally, this guidance is broken down into dosimetric and non-dosimetric testing procesured.
Non-dosimetric TPS Commissioning
Accurate image interpretation
- Spatially accurate with respect to distance and orientation
- Accurately converts CT number to physical or electron density
- Accurate representation of machine parameters
Beam energy spectrum and profiles are correctly modeled
- Beam modifiers such are collimation, MLC, wedges, and applicators are correctly modeled
- TPS is able to accurately compute the impact of immobilization devices and bolus
- Accurate presentation of anatomical and dosimetric calculations
Accurately localizing and computing contour areas
- Producing accurate anatomical dose volume histograms (DVH)
Dosimetric TPS Commissioning
TPS ability to recreate input data
- When TPS is used to compute the same geometry data used in commissioning, it produces an accurate recreation
Algorithm verification
- Algorithm verification refers to the process of determining that the algorithm operates as intended. This does not need to be done at every clinic because it is a test of the algorithm's function rather than specific implementation.
Calculation verification
- Calculation verification means testing that the TPS accurately computes the dose distribution of a given plan delivered by a given machine for a variety of circumstances including
- Irregular field shapes
- Heterogeneous materials (i.e. lung, bone)
- Differing SSDs
- Wedges
- MLC shaped fields
- Dynamically shaped fields (i.e. Sliding window IMRT, VMAT)
Evaluation of limiting cases
- Determining what limiting cases should be tested requires both understanding the TPS weaknesses and outlining the use scenarios for a given application.
- Limiting cases include
- Large and small SSD
- Large and small fields
- Situations where the algorithm is likely to be weak
End-to-end testing
- End-to-end testing takes a phantom from simulation to dose calculation and measured the final delivered dose to assure integrity through the entire treatment process.
- End-to-end testing often makes use of an anthropomorphic phantom which simulates human geometry.
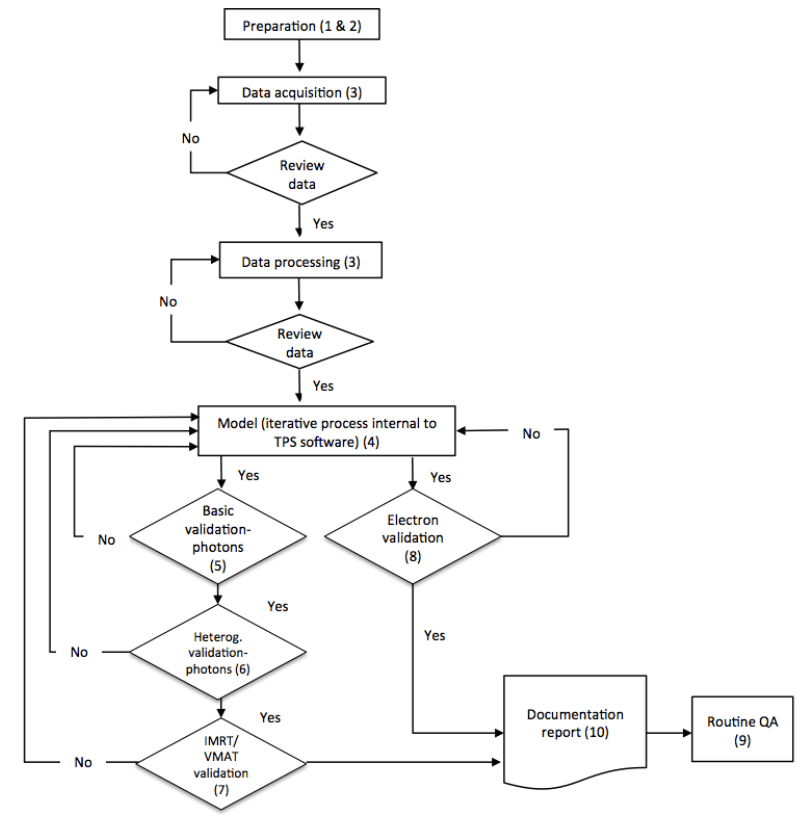
AAPM Medical Physics Practice Guideline 5 Methodology
AAPM MPPG5.a presents TPS commissioning and quality assurance as a three phase process.
TPS Commissioning And QA Phases
- Data Acquisition and Processing
- During the first phase of commissioning, physical measurements must be made and analyzed for use in the treatment planning system.
- Attention to detail here is critical as errors can lead to significant systematic error and potential consequences for patients under treatment.
- Data acquisition is the subject of AAPM Medical Physics Practice Guideline 5.a: Commissioning and QA of Treatment Planning Dose Calculations - Megavoltage Photon and Electron Beams (External Link).
- TPS Validation and Beam Model Iteration
- During the second phase of commissioning, the physical measurements are applied to the TPS software to produce a model.
- This model is then tested against additional physical measurements in a variety of simulated real use cases.
- Results of this testing are used to iteratively refine the model.
- This section is the primary focus of AAPM TG-106: Accelerator Beam Data Commissioning Equipment and Procedures (External Link)
- Ongoing Quality Assurance
- Finally ongoing quality assurance is assures that the software's beam model remains valid into the future.
- Checksum files are used to assure no changes to software configuration has occurred.
- Physical measurements tested against baseline measurements are also used.
Key Point: MPPG 5 is not applicable to the following:
- Systems that do not use an MLC for beam shaping
- Commissioning of small field TPS systems (field sizes <2x2cm2)
- Use of non-commercial TPS systems
- Sub-MV or bachytherapy TPS systems
- Non-dosimetric components of TPS systems (e.g. biological response models, dose-volume histograms, image registration or contouring, etc)
Phase 1: Data Acquisition and Processing
CT Calibration Data
CT calibration in the TPS consists of specifying what CT number (Hounsfield Unit) corresponds to what electron or physical density.
Equipment
CT number to density phantom consisting of materials with known physical and electron density.
Density range: Air (~0.001 g/cm3) to dense bone (1.4-1.9 g/cm3). High density materials such as titanium and gold may also be required depending upon clinical use.
Process
- CT density phantom is scanned on CT using standard kVp setting.
- Measure mean CT number within each density plug.
- Create table correlating CT number to electron/physical density within the TPS.
Additional Readings
AAPM TG-66: Quality assurance for computed-tomography simulators (External Link)
Treatment Beam Data
Although MPPG5.a notes the need for proper data acquisition and processing, it largely refers the reader to AAPM TG-106 for information on basic beam data collection.
Note: Although inhomogeneity characterization is important to the TPS commissioning process, it is considered beyond the scope of AAPM TG-106.
Data Required for Beam Model Creation
Minimum Recommended Photon Beam Data
- Percent Depth Dose (PDD)
- Field profiles (in-plane and/or cross-plane) as various depths
- MLC data
- Interleaf leakage
- Intraleaf leakage
- Tongue and Groove
- Head leakage
- Total scatter
- Tray factors (if used)
- Wedge factors
Minimum Recommended Electron Beam Data
- Percent Depth Dose (PDD)
- Field profiles (in-plane and/or cross-plane) as various depths
- Cone factors
- Insert factors
- Virtual source position
- Found using profile scans in air
IMRT/VMAT Data
Most commercial treatment planning systems extrapolate basic beam measurements to produce their small field dose distributions. Therefore, small field, IMRT, and VMAT measurements are made for the purpose of beam model validation rather than model creation.
MPPG5.a recommended measurements
- Percent depth dose profiles for field sizes down to 2x2cm2
- Small field output factors (down to at least 2x2cm2)
- MLC intraleaf and interleaf transmission, leaf gap
- Use small ion chamber under leaf
- Use film for interleaf leakage
- Leaf tip penumbra profile
- Use small detector (diode of micro-chamber)
- Leaf timing for binary MLC systems
- E.g. Tomotherapy
Evaluation Comparison
All data should be compared to a reference data set from as similar a treatment machine as possible. The intent of this check is to identify potential changes in beam inverse square effect, beam divergence, beam energy, and others. Such changes may indicate an error in measurement and should be closely reviewed prior to inputting the data into the TPS. Data to be compared includes:
- Crossbeam profiles at multiple depths and field sizes
- Percent depth dose distributions for varying field sizes
- MLC transmission factors
Additional Readings
AAPM TG-106: Accelerator Beam Data Commissioning Equipment and Procedures (External Link)
Phase 2: Beam Model Creation
For the purpose of validation and fine tuning, MPPG5.a considers each "configured beam" to by distinguished by a unique energy and treatment head configuration. For example; 6MV, 6MV small field/SRS, 6MV Flattening Filter Free, and 6MV with physical wedge are all considered unique beams requiring individual validation.
AAPM MPPG 5 breaks down validation into 4 categories, listed below, and advocates for an iterative process of validation and model tuning.
Validation Categories
- Basic Photon Dose Calculation
- Photon Dose Calculation in Heterogeneous Media
- Photon Dose Calculation in IMRT/VMAT Setting
- Electron Dose Calculation
Beam Model Parameters
Photon Parameters
The below parameters are commonly used in Kernel based dose computation algorithms.
Photon Energy Spectrum
The energy spectrum is commonly modeled as a set of descrete energies. This is because each energy commonly has a unique, monte carlo generated, dose deposition kernel.
Photon energy spectrum fit is dominated by PDD fitting, often with a focus on the reference field size (i.e. 10x10cm2).
Electron Energy Spectrum
Electron contamination of the photon beam must be modeled for accurate dose calculation in the superficial region. Because there is no Kernel for electron dose distribution, a continuous energy distribution may be used.
Electron fitting focuses on the superficial region of the PDD curves.
Primary Source Geometry
The location and shape of the primary photon source is important for accurate ray tracing.
Source location: Taken to be the physical location of the target in the treatment head.
Source profile: May represent a physical source size or may be optimized to fit small field measurements. The profile is often represented as a circular or elliptical Gaussian.
Typically 0.5-3mm diameter.
Off-axis Softening
Because of differential attenuation within the flattening filter, flattened clinical beams are soften (become lower in mean energy) with increasing radial distance from the beam axis. This causes the lateral portions of a clinical beam to attenuate more rapidly than the central portions. This effect must be modeled in software.
Off-axis softening optimization focuses on large field profiles at depth near dmax in the 90-100% of maximum dose range.
Collimation (Jaw and MLC) Parameters
The treatment planning system must accurately model position and attenuation of the collimation devices used in planning.
Positioning: Positioning is typically optimized by matching the full-width-at-half-max value at the set SSD (typically 100cm).
Attenuation: Attenuation is found averaging large out of field, blocked, measurements.
Output Factor Corrections
Output factor corrections may be used for variable field sizes and beam modifier such as dynamic or physical wedges.
Why output factor corrections with Ray-Tracing and modeled attenuation?
Ray-tracing follows the beam path from a voxel back to the source and includes the impact of attenuation. These effects are NOT included in TPS output factor corrections. Rather, these corrections account for differences in scatter counts to the monitor chamber. Changes in the number of these scatter counts influences when the monitor chamber shuts off the beam and this effect is modeled using output factor corrections.
For example, the jaws smaller fields scatter more electrons back into the monitor chamber. This causes the monitor chamber to read more dose than is actually delivered. In effect, the monitor chamber shuts off the beam "early" for smaller fields.
Key Point: Beam model parameters vary from vendor-to-vendor and, hence, is not extensively covered in MPPG 5. OMP presents only a set of common parameters and their impact dose calculation.
Basic Photon Dose Calculation Tests
All basic photon dose calculation tests are computed and measured in unit density phantoms with simple beam arrangements.
Barely meeting tolerances in this section may result in tolerance failures during heterogeneity or IMRT/VMAT testing. It is recommended, therefore, that some model adjustment be made to optimize the results of this section even if the model is already within tolerance.
Key Point: There are two categories of basic photon dose tests.
- Tests comparing the TPS model to data used directly in commissioning.
- Tests comparing the TPS model to plan measurements that vary by a small number of variables from commissioning data plans.
Comparisons between TPS model and data used in commissioning
5.1 Dose Distribution in planning module vs modeling (physics) module
Purpose: To assure that the beam model is identical between TPS modules
Test: Compare planning module dose calculation to physics module dose calculation for the same large (>30x30cm2) field in simulated water.
Tolerance: Identical
5.2 Dose in test plan vs clinical condition
Purpose: Confirm that the TPS can accurately reproduce simple reference beam measurements.
Test: The TPS should calculate dose to the reference point using beam calibration conditions (I.e. TG-51). TPS calculation should be compared to the measured data used in TPS commissioning.
Tolerance: 0.5%
5.3 Dose distribution calculated in planning system vs commissioning data
Purpose: Confirms that planning module dose calculated in water phantom matches commissioning data.
Test: Calculate dose for large and small field commissioning data in planning module. Compare calculated PDD and off-axis ratios to commissioning data.
Tolerance: 2%
Comparisons between TPS model and homogeneous non-commissioning data
Tests in this section continue to compare TPS calculation to measurement for water phantoms but now the physical measurements are not directly used in commissioning the beam model. These plans change only a small number of parameters from commissioning plans.
| Test | Sample Test from: IAEA TRS-430 (External Link) |
| 5.4 Small MLC-shaped field (non-SRS) | Photon Test 1 |
| 5.5 Large MLC-shaped field with extensive blocking (e.g. mantle) | Photon Test 3 |
| 5.6 Off-axis MLC shaped field, with maximum allowed leave over travel | Photon Test 2 |
| 5.7 Asymmetric field at minimal anticipated SSD | Photon Test 6 |
| 5.8 10x10cm2 field at oblique incidence (≥20°) | Photon Test 10 |
| 5.9 Large (>15cm) field for each nonphysical wedge angle | None |
Remembering MPPG5.a Basic Dose Calculation Tolerances
| Condition | Tolerance |
| Comparing calculations different TPS modules (Test 5.1) | Identical |
| Reference dose per MU (Test 5.2) | 0.5% |
| High dose region:
≤1 parameter changes between test conditions and reference data conditions |
2% |
| High dose region:
>1 parameter changes between test conditions and reference data conditions |
5% |
| Penumbra region | Distance to agreement: 3mm |
| Low-dose tail | 3% of maximum field dose |
Photon Dose Calculation in Heterogeneous Media
Validation of photon dose calculation in heterogeneous media has two parts:
- Direct validation that the system correctly maps physical or electron density in a planning CT.
- Validating that dose is correctly calculated in the following areas
- Within low density tissue
- Near the interface of heterogeneous tissues (low and high density)
- Beyond the heterogeneous tissues (low and high density)
Recommendations for dose validation in heterogeneous media
- A 5x5cm2 field size is recommended because small fields enhance the dosimetric impact of low-density materials.
- Measurements should not be made directly at the interfaces of inhomogeneities because these are build-up/build-down regions.
- The inhomogeneity should cause at least a 10% dose correction compared to the homogeneous phantom.
- Edits to the beam model as a result of failures in this section require repeated validation of the basic photon calculation tests.
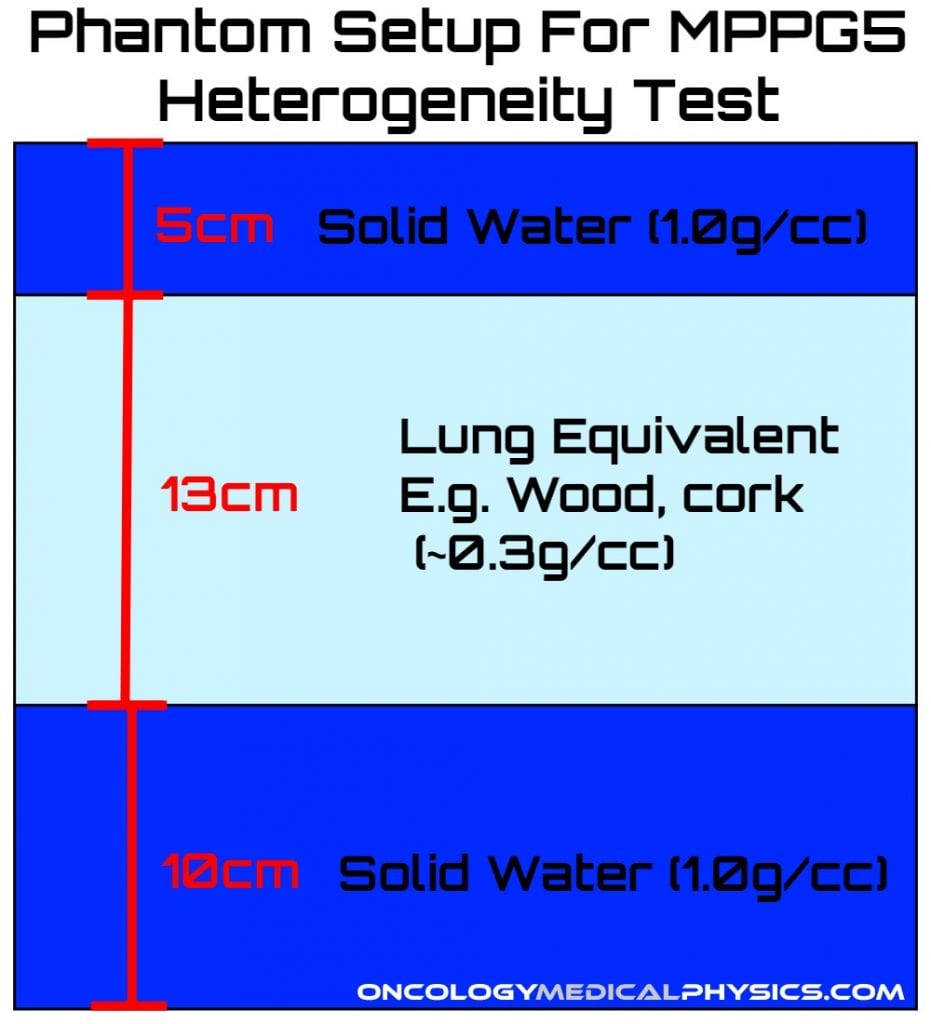
| Test | Description | Tolerance |
| 6.1 Validate planning system reported physical or electron density. | CT-density calibration for air, lung, water, dense bone, and other tissue types. | - |
| 6.2 Heterogeneity correction distal to lung tissue. | Calculate and measure dose above and below a lung density inhomogeneity. | 3% |
Photon Dose Calculation in IMRT/VMAT Setting
IMRT/VMAT validation tests recommended in AAPM MPPG5.a draw heavily from AAPM TG-119.
Recommendations for dose validation in IMRT/VMAT setting
- Field sizes down to at least 2x2cm2 must be investigated even if such data is not required by the TPS.
- AAPM TG-119 found that agreement to within 3% of prescription dose is generally appropriate.
- 2%/2mm gamma index evaluation is recommended over the more common 3%/3mm because it is able to more readily identify areas of concern.
- Investigation should focus on highly modulated IMRT/VMAT plans as these will be most impacted by subtle errors in MLC model parameters.
- There is significant disagreement in the the required testing for an IMRT/VMAT program. MPPG5 tests recommend only the minimum and more testing may be appropriate in a given clinical setting.
IMRT/VMAT TPS Validation Tests
| Test | Description | Recommended Detectors |
| 7.1 Verify small field PDD | Plan and measure PDD for fields at least as small as 2x2cm2 | Diode detector Plastic scintillator |
| 7.2 Verify small MLC defined field output factors | Use small MLC defined fields | Diode detector Plastic scintillator Mini/micro-ion chamber |
| 7.3 TG-119 tests | Head-and-neck and C-shaped test plans recommended | Ion chamber Film Detector array |
| 7.4 Clinical Tests | At least 2 clinically relevant cases should be planned, measured, and an in-depth analysis should be performed. | Ion chamber Film Detector Array |
| 7.5 External Review | Simulate, plan, and treat an anthropomorphic phantom with embedded dosimeters.
Most commonly, this is performed using the IROC Houston Head and Neck tests as well as the Thoracic tests. If IROC testing is not possible, the minimal acceptable validation is to have another Qualified Medical Physicist perform and independent evaluation. |
Anthropomorphic phantom with embedded dosimeters |
IMRT/VMAT TPS Validation Test Tolerances
| Measurement Method | Region Investigated | Tolerance |
| Ion Chamber | Low-gradient (uniform dose) region | 2% of prescribed dose (Targets)
3% of prescribed dose (Regions/Organs-at-Risk) |
| Planar/Volumetric Detector Arrays | All Regions | No tolerance
Note: The 2%/2mm gamma index should be investigated but not pass rate tolerance is recommended. |
| End-to-end testing | Low-gradient (uniform dose) region | 5% prescribed dose |
Electron Dose Calculation
Electron validation is relatively simple compared to a full photon validation. Important aspects of electron dosimetry and treatment planning are noted by AAPM TG-25 and AAPM TG-70.
AAPM TG-70 states that electron beam treatment planning should be:
- CT based
- Employ 3D heterogeneity correction
- Use a pencil beam algorithm or better
Recommendations for electron dose validation
- Create plots of PDD and output factors for all standard cutout sizes at each energy.
- This is used to confirm correct qualitative behavior of energy and field size.
- Clinical use of non-routine electron fields (e.g. abutting fields, small fields, etc) will require additional verification to understand the limits of the electron model.
Electron TPS Validation Tests
| Test | Description | Tolerance |
| 8.1 Basic model verification with shaped fields | Measure PDD and output factor for cutouts at standard and extended SSDs. | 3%/3mm |
| 8.2 Surface irregularities obliquity | Oblique incidence using reference cone and nominal SSD. | 5% |
| 8.3 Inhomogeneity test | Use reference cone and SSD in heterogeneous phantom. | 7% |
Phase 3: Ongoing Quality Assurance
Once TPS commissioning and validation is complete, the final step is to create an ongoing quality assurance program which achieves the following goals:
- Verifies that the TPS remains in the commissioned configuration.
- This may be accomplished using a "check sum" file
- Verifies that the TPS continues to correctly calculate dose following and TPS upgrades.
- This is a comparison of calculated doses after commissioning to post TPS upgrade calculated dose.
- Calculations should be compared at the 1%/1mm level.
- Selected plans should be compared for all commissioned beams.
What is a checksum file?
A checksum is a small unique code derived from a large data set. A checksum created from the original commissioned data set can be compared to a new checksum file during routine quality assurance. If both checksum files are the same, it is safe to conclude that the commissioned data has not been edited.
Navigation
Not a Premium Member?
Sign up today to get access to hundreds of ABR style practice questions.