IMRT Quality Assurance
Background
Intensity modulated radiotherapy (IMRT) treatment plans rely on many small and irregular fields to produce complex dose distributions. These irregular fields present challenges both in producing accurate dose calculations and in the ability of treatment machines to reliably produce the desired fields. Additionally, IMRT planning is chosen to allow dose escalation, as compared with a 3-dimensional plan, by avoiding nearby healthy anatomical structures. These factors necessitate the measurement of the computed dose distribution to assure that target structures receive adequate dose and healthy tissue is avoided.
Downloads
AAPM TG-230: Dosimetry Tools and Techniques for IMRT (external link)
AAPM TG-218 – Tolerance Limits and Methodologies for IMRT Measurement-Based Verification QA (external link)
IMRT Quality Assurance Process
1. Plan is approved by the supervising radiation oncologist.
2. The treatment plan, which consists of MLC leaf sequences as a function of gantry angle and delivered monitor units, is used to calculate the expected dose distribution to a phantom.
3. The phantom is irradiated, and the dose distribution is measured.
4. Measured dose distribution is compared with the phantom calculated dose distribution, most often using the γ-index.
5. Plans achieving an acceptable agreement between measurement and calculation are approved for delivery. Plans with unacceptable agreement are evaluated and may be replanned or remeasured.
Key Point: The utility of a physical measurement compared with an additional computation using the treatment machine’s log files is debated in the field of medical physics. Despite this, a physical phantom-based measurement remains that standard most often employed.
Verification Metrics
Agreement between measured and calculated dose is usually compared on a point-wise basis, evaluating both the absorbed dose and the location.
Dose Difference
Dose difference directly compares the measured dose at each point to the corresponding calculated dose at that point. Criteria based on dose difference often normalize the dose difference to either the local dose calculated dose or the maximum calculated dose. Dose difference works very well in areas of uniform dose but can produce high failure rates within dose gradients due to errors of alignment between the measured and calculated dose.
Key Point: Dose difference evaluated using the global maximum for normalization will produce higher pass rates, especially in the low dose regions, than those using local dose for normalization.
Distance-to-Agreement
Distance-to-agreement (DTA) tests measure the distance between a point on the measured dose distribution and the nearest point on the calculated distribution with equal dose. Unlike dose difference tests, DTA tests work well in evaluating regions of high dose gradient but becomes over-sensitive in regions homogeneous dose.
Key Point: Distance-to-agreement test are sometimes referred to as Van Dyk tests because of an influential 1993 paper.
Dyk, J., Barnett, R., Cygler, J., & Shragge, P. (1993). Commissioning and quality assurance of treatment planning computers. International Journal of Radiation Oncology Biology Physics, 26(2), 261–273. https://doi.org/10.1016/0360-3016(93)90206-b
γ-Index
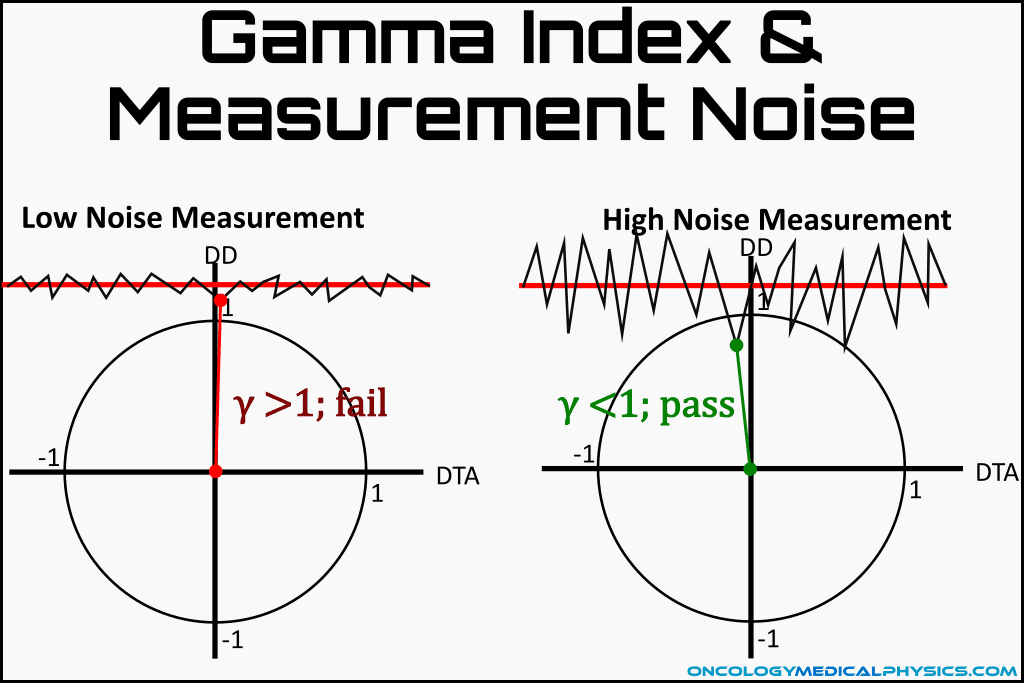
Gamma index attempts to combine dose difference and DTA into a single metric that is useable in both areas of dose gradient and homogeneous dose. The gamma test defines a 2-dimensional space with one axis being dose difference and the other being distance-to-agreement. Γ is computed as the Euclidean distance, normalized to passing criteria, for each point. The minimum value of Γ for a point is taken to be γ and is used for evaluation.
![]()
![]()
Points with a γ-index value greater than 1 fail the tests. A plan evaluated against the gamma index will be considered clinically acceptable if the percentage of all points with minimum gamma index of less than 1 is greater than a threshold value, usually 90% or 95%.
γ-Index Normalization
The calculated dose difference is expressed as a percentage of the normalization dose. The normalization dose are chosen as either the local maximum dose (which normalizes to the dose at the corresponding point in the reference distributions) or the global maximum dose in the reference distribution.

AAPM TG-218 recommends use of a global normalization for IMRT QA, noting that it is more clinically relevant than a local normalization. The local normalization is more stringent and may be more applicable to commissioning tasks.
γ-Index Threshold Dose
Very low dose regions are often not clinically relevant and may be somewhat inaccurately calculated by the treatment planning system. Further, inclusion of these points would greatly reduce the rigor of gamma index tests when using global normalization. Therefore, a threshold dose is defined and point with absorbed dose lower than the threshold value are not evaluated.
AAPM TG-218 recommends a threshold dose of 10% of the global maximum.
Gamma Index
Key Points:
- Dominated by dose difference in homogeneous regions
- Dominated by distance-to-agreement in heterogeneous regions
- Commonly evaluated using:
- Distance criteria of 2-3mm
- Dose difference criteria of 2-5% (3% is most common)
- Pass rate criteria of 90% or 95%
- Threshold dose of 10%
Limitations of γ-Index
- Gamma index is less stringent than dose difference in homogeneous regions.
- Gamma index is less stringent than DTA in high dose gradient regions.
- Gamma index is made less stringent high noise measurements.
Tolerance and Action Limits
Once agreement between measured and calculated dose is compared using a verification metric, the course of action must be determined. AAPM TG-218 recommends the use of tolerance limits and action limits to determine which course of action should be taken.
Tolerance Limits
Tolerance limits bound the normal variability of the treatment machine and plan type. Measurements falling below the tolerance limit are considered to be within the normal operation of the system. Measurement falling outside of the tolerance limit indicate a potential problem with the specific plan, treatment system, or treatment planning system. The intention of a tolerance limit is to find errors in the treatment system or treatment planning system before they result in unacceptable errors that exceed action limits.
Actions taken for measurements outside the tolerance limit:
- Assess the cause of the deviation
- Measurement error
- Plan undeliverability
- Changes to machine or TPS parameters
- Evaluated the plan against the action limit to determine if it is clinically acceptable
Action Limits
Action limits define the amount of measurement deviation allowed without risking harm to the patient. Failure to meet action limits will result in either creation of a new treatment plan or the acceptance of the plan based on the unique circumstances of the patient.
AAPM TG-218 Tolerance and Action Limit Recommendations
Tolerance Limits: γ pass rates should be ≥95% using 3%/2mm tolerance and 10% threshold.
Action Limits: γ pass rates should be ≥90% using 3%/2mm tolerance and 10% threshold.
Key Point: Tolerance limits are generally tighter (require higher pass rates, use lower DTA or dose difference threshold) than action limits. Plans failing to meet the tolerance limit may be clinically acceptable while those failing to meet the action limit may risk harm to the patient.
Measurement Devices
Single Point Measurement
The simplest patient specific measurement system consists of a single dosimeter placed within a phantom. Small volume ionization chambers (0.6cc to 0.007cc) are the most commonly chosen dosimeter but diode detectors, MOSFET detectors, plastic scintillators, and others could be used. Single point measurements work well for small treatment volumes and uniform dose but provide limited utility for large complex treatment volumes. Single point measurements may be made as a supplement to 2-dimensional film measurements which have excellent spatial resolution but require careful calibration to achieve accurate absolute dose measurements.
Two-Dimensional Measurements
Two-dimensional (2D) measurements provide both dosimetric and spatial information allowing use of the γ-Index for delivery evaluation.
Common Types of 2D Detectors
- Film
- Ion chamber arrays
- Diode arrays
- Electronic Portal Imaging Devices (EPIDs)
Three-Dimensional Measurements
True three-dimensional (3D) detectors provide a measurement throughout the irradiated volume but are uncommon in clinical practice due to their difficulty of use. As one example, BANG gel detectors must read out by performing an MRI or optical CT scan on the gel after irradiation.
Quasi-3D detectors fall into two categories, detector arrays arranged around a cylinder and use of multiple orthogonal planar detector arrays. These detectors provide more information about the 3D dose distribution than a planar array without sacrificing ease of use.
Quasi-3D Detectors
- Detectors arranged around the surface of a cylinder
- Multiple orthogonally oriented planar detectors
True 3D Detectors
- Gel polymers
- Polyurethane embedded leuco dye
Navigation
Not a Premium Member?
Sign up today to get access to hundreds of ABR style practice questions.