Gynecological Brachytherapy
Treatment Regimen
Low Dose Rate: The Manchester System
LDR alone (Stages IA1-IB1): 50-70Gy prescribed to point A
LDR as boost for external beam (Stage IB1 – IV): 30-40Gy to point A for a total including external beam of 85-90Gy
High Dose Rate Prescriptions
Cervical Cancer
Early stage:
20-45Gy external beam therapy followed by 30-45Gy in 5 to 8 fractions of brachytherapy.
Late stage:
45-50.4Gy external beam therapy followed by 28-35Gy in 4 to 6 fractions of brachytherapy.
Uterine Cancer
(Post Operative)
Brachytherapy Alone:
3 to 5 fractions of 7 to 4.7Gy prescribed to a depth of 5mm or 3 to 5 fractions of 10.5 to 7.5Gy prescribed to vaginal surface.
Brachytherapy following external beam:
2 fractions of 5.5Gy prescribed to a depth of 5mm or 2 fractions of 8Gy prescribed to vaginal surface.
Uterine Cancer (Inoperable)
Brachytherapy Alone:
4 to 7 fractions of 8.5 to 5.7Gy prescribed to a depth of 2cm.
Brachytherapy following external beam:
45Gy external beam followed by 2 to 4 fractions of 8.5 to 5.2Gy brachytherapy prescribed to a depth of 2cm.
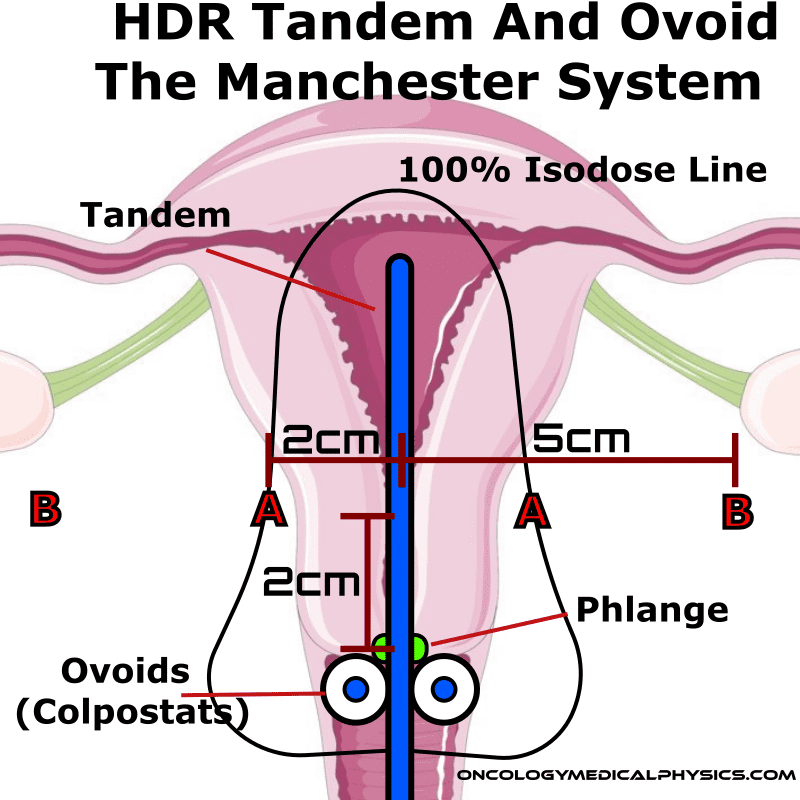
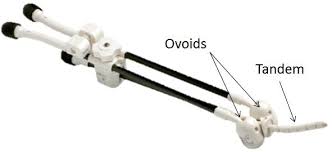
Tandem and Ovoid
Tandem and Ovoid (T&O) treatments are used to treat the cervix, uterus, and upper 1-2cm of the vagina. Tandem and Ovoid applicators, such as the Fletcher Suite applicator, consist of a central tandem inserted through the cervical os and into the uterus and two ovoids (colpostats) which are placed in the left and right vaginal fornices. A phlange prevents the over-insertion of the applicator which could otherwise result in perforation of the uterine wall.
Dose Reporting: The Manchester System
The manchester system is a system of dose reporting based on dose at positions relative to the applicator and surrounding anatomy.
Point A
This point is 2cm superior to the phlange (cervical os) and 2cm lateral to the tandem midline.
Point A is a common prescription point corresponding, approximately, to the point where the uterine vessels cross the ureter. Radiation tolerance is of these structures are thought to be the main limiting factor in irradiating the uterine cervix.
Point B
Point B is another dose reporting point located 5cm lateral from the patient's midline.
Point B is intended to be representative of the pelvic lymph node dose, hence its definition relative to the patient’s midline rather than the tandem’s midline.
Bladder Point
Bladder Point is the point of highest dose in the bladder.
Bladder dose should be less than 80% of dose to point A.
Rectal Point
Rectal Point is the point of highest dose in the rectum.
Rectum dose should be less than 80% of dose to point A.
Key Point: Point A is defined relative to the midline of the tandem while point B is defined relative to the midline. This is because point A (which represents the crossing of the uterine artery and the ureter) is best approximated relative to the uterus while point B (which represents the pelvic lymph nodes) is best approximated relative to the patient's body. This difference can be significant when the uterus is tilted relative to the pelvis.
High Dose Rate Tandem and Ovoid
High dose rate tandem and ovoid treatment mimic the dose distribution of LDR treatments. However, incorporation of image guidance allows for better tailoring of exact dose distribution and more detailed dose reporting.
GYN GEC-ESTRO Recommendations
As gynecological brachytherapy transitioned from LDR to HDR, GEC-ESTRO wisely put together a working group to standardize dose reporting. This new system leverages improved use of imaging and computerized treatment planning.
Structures (GYN GEC-ESTRO Working Group I)
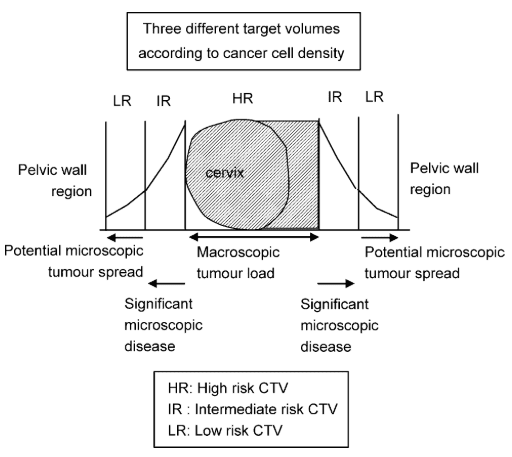
GTV (Gross Tumor Volume)
Includes macrscopic tumor extension as detected by clinical examiniation and visualized on MRI.
HR CTV (High Risk Clinical Target Volume)
Includes whole cervix and presumed extracervical tumor extent.
Additional disease extent may be determined by palpation, direct visualization, or on MRI/CT imaging.
HR CTV should receive full dose.
IR CTV (Intermediate Risk Clinical Target Volume)
Includes the GTV, HR CTV plus a safety margin of 5-15mm to account for significant microscopic residual tumor load.
IR CTV should receive at least 60Gy.
LR CTV (Low Risk Clinical Target Volume)
Subscripts
D = at time of diagnosis. (E.g. GTVD is the GTV at time of diagnosis)
B# = at time of brachytherapy treatment. (E.g. GTVB1 is the GTV at time of first brachytherapy treatment)
Dose Reporting (GYN GEC-ESTRO Working Group II)
The following items should be reported for a GYN brachytherapy case.
- Prescribed dose
- Total Reference Air Kerma (TRAK)
- Dose to Point A (left, right, and mean)
- D100% and D90% for GTV, HR CTV, and IR CTV
- Dose to bladder and rectum ICRU 38 reference points
- D0.1cc, D1cc, D2cc for organs at risk (rectum, sigmoid colon, bladder, and vagina)
- D5cc, D10cc if contouring organ walls is performed
- Biologically weighted doses (EQD2)
MR Guided Contours (GYN GEC-ESTRO Working Group IV)
- A T2 weighted MRI is used in contouring as it allows for proper visualization of the tumor, cervix, bladder, vagina, rectum, and sigmoid colon.
- A T1 weighted image may also be used but may be useful in determining the extent of nodal involvement.
- The image should be oriented para-axial (orthogonal to the urterine axis) and para-sagital and para-coronal (parallel to the uterine axis).
- 0.1T to 3T MR scanners are acceptable with 1.5T being the norm.
- SNR increases with strength but spatial linearity and inductive heating become a limiting factor at high fields.
- Consistent bladder filling is an important parameter in treatment planning.
- A foley catheter is inserted and the bladder is first drained then filled with ~7cm3 of either diluded gadolinium contrast of saline solution.
- MR compatible applicators may either be constructed of plastic or titanium.
- Titanium applicators will induce susceptibility artifacts.
- The low visibility of plastic on MR scans may require Gadolinium doped dummy wires to be inserted into the channels allowing for proper reconstruction.
- Applicator should be fixed in place by packing the vagina with cotton gauze. This prevents applicator motion between simulation and treatment.
Tandem and Ring
Similar to T&O, the Tandem and Ring (T&R) applicator is able to deliver a wider and more Anterior/Posterior dose distribution compared. T&R may be appropriate for larger tumors, increased upper vaginal involvement, or pelvic side wall invasion.
Rotte Applicator
The Rotte Applicator is “Y” shaped but produces a “pear” shaped dose distribution useful for treating some cervical anatomies.
Vaginal Cylinder
Vaginal cylinders are cylindrically shaped applicators used in the treatment of vaginal disease. They may have a single central channel or their may be multiple channels nearer to applicator surface allowing for more control over the dose distribution.
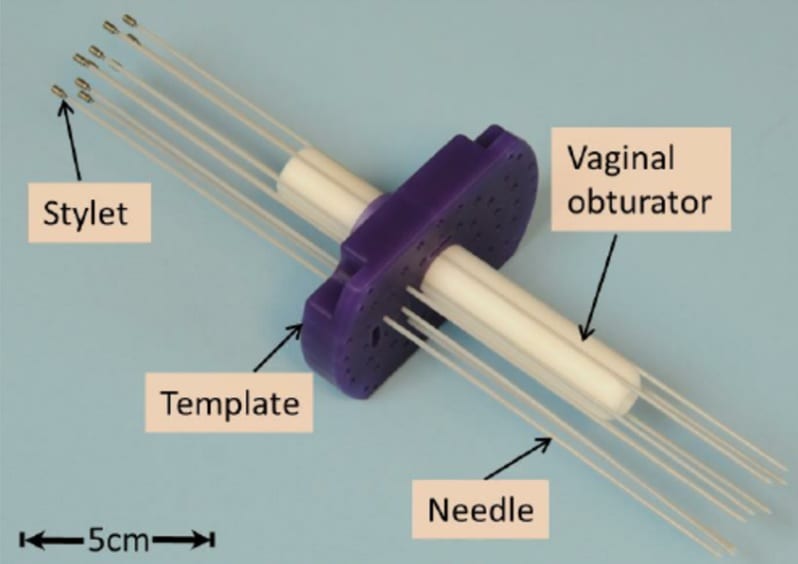
Syed and Interstitial Needles
Interstitial needles are often used in gynecological brachytherapy as a supplement to one of the above applicators. They may be used to improve coverage to areas more distal to the vagina, uterus, or cervix.
One common applicator template is the Syed/Neblett GYN template. This design features a central cylinder (obturator) and lateral needle holes.
Navigation
Not a Member?
Sign up today to get access to hundreds of ABR style practice questions.