Total Skin Electron Therapy
Overview
As presented in AAPM TG-30, the goal of total Total Skin Electron Therapy (TSET) is “to treat virtually the entire body surface to a limited depth and to a uniform dose using electrons with a low X-ray background.” TSET is most commonly prescribed in the treatment of Mycosis Fungoides and is highly effective. Although the common treatment techniques were developed in the early 1950s, they see continued use today because of their safety and efficacy.
Downloads
AAPM TG-30: Total Skin Electron Therapy - Technique and Dosimetry (External link)
AAPM TG-25: Clinical Electron-Beam Dosimetry (External link)
Mycosis Fungoides
Mycosis Fungoides (MF), sometimes called Sezary syndrome, is a low grade non-Hodgkin T-cell lymphoma of the skin. In advanced stages MF may involve the lymph nodes, blood, and visceral organs.
- Typical Age at diagnosis: 45-69 years.
- Incidence: Approximately 3 in 10.
- Disease progression:
- Begins as a scaly red rash in areas not exposed to the sun.
- Path Phase is marked by small areas of raised bumps and hardened lesions.
- In Tumor Phase MF presents itself as raised tumors on the skin.
Treatment Options
Treatment options are dependent upon the extend of disease requiring either local control or treatment of extensive disease.
Local control options
- Topical Corticosteroids or Chemotherapy
- UV photon therapy
- Local Radiation: electron or orthovoltage X-ray
- Typical prescription: 20-30Gy in 1.2-2Gy/fraction
Extensive disease options
- Total skin electron therapy (TSET)
- Typical prescription: 30-36Gy surface dose over 6-10 weeks
- Highly effective treatment option with complete response rates of 95% for T1 to 75% for T4.
Total Skin Electron Therapy Treatments
Treatment Parameters Per Guidelines
Prescriptions
- Standard course: Deliver at least 26Gy to a depth of 4mm over 6-10 weeks.2 This requires 31-36Gy surface dose.
- Shorter course: 12Gy in 3 weeks.
Field Parameters
- Energy: 3-7MeV (at patient), 4-10MeV (at beam window)1
- SSD: 3-8 meters
- Field size at patient: 200cm by 80cm1
Field Inhomogeneity or Uniformity
- EORTC Consensus:
- <10% dose inhomogeneity to air at treatment distance2.
- AAPM TG-30:
- ± 8% vertically over central 160cm
- ± 4% horizontally over central 80cm
Penetration and dose fall off
- EORTC Consensus:
- 80% isodose line must be at least 4mm from skin surface
- 20% isodose line should be <20mm from skin surface
- AAPM TG-30:
- 50% isodose line should be 5-15mm
Maximum Dose
- 120%, may require shielding to achieve2
Photon contamination
- EORTC Consensus
- Total dose to marrow from photons should be <0.7Gy
- AAPM TG-30
- <4% (1.6Gy)
Sources
1. AAPM Task Group 30. Total Skin Electron Therapy: Technique and Dosimetry. AAPM; 1987:58.
2. Total skin electron radiation in the management of mycosis fungoides: Consensus of the European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project Group. J Am Acad Dermatol. 2002 Sep;47(3):364-70.
Six Dual Field (Stanford) Technique
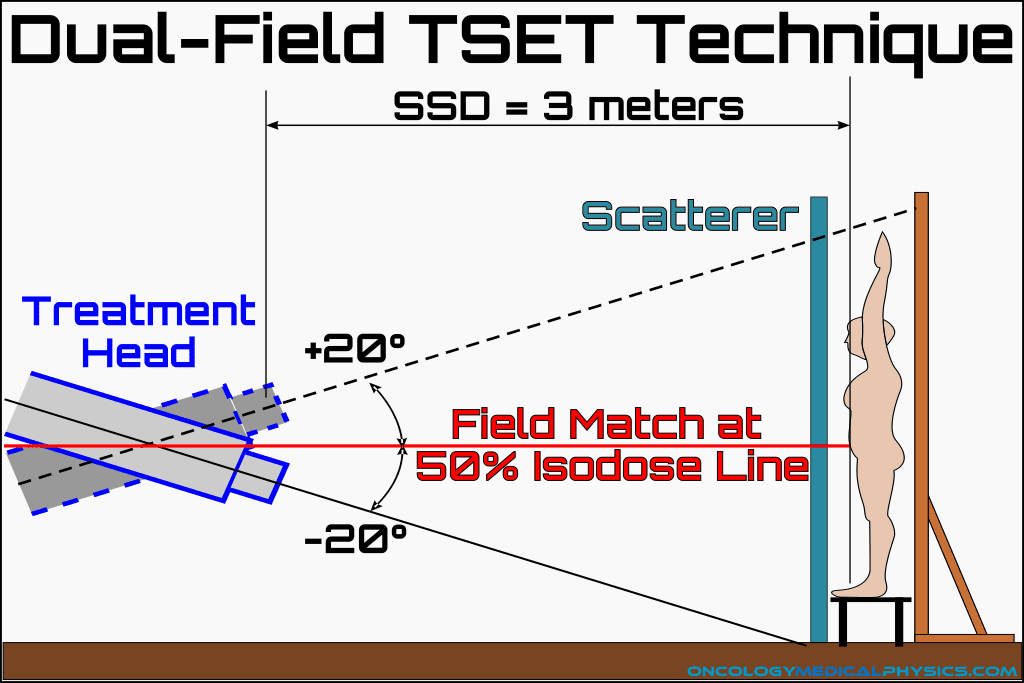
The stanford TSET technique uses 6 dual-fields. Each dual-field consists of one field angled up at about 20 degrees and another angled down at about 20 degrees such that the up and down fields match at the 50% isodose line at height of isocenter. A source-to-surface distance of 3-7 meters is usually sufficient to cover the patient with a uniform field size of 200cm by 80cm.
Important Field Points
- Angling the field’s central axis above the head and below the feet reduced Bremsstrahlung X-ray contamination.
- Bremsstrahlung X-rays are predominantly forward directed.
- Angles of approximately 20 degrees relative to horizontal.
- Because many electrons enter the body obliquely, electrons penetrate less deeply than the 2cm per MeV in water approximation.
- Field energy at accelerator must be 1-2MeV higher than at the patient surface because electrons loose approximately 1MeV of energy every 4 meters in air.
Patient Setup
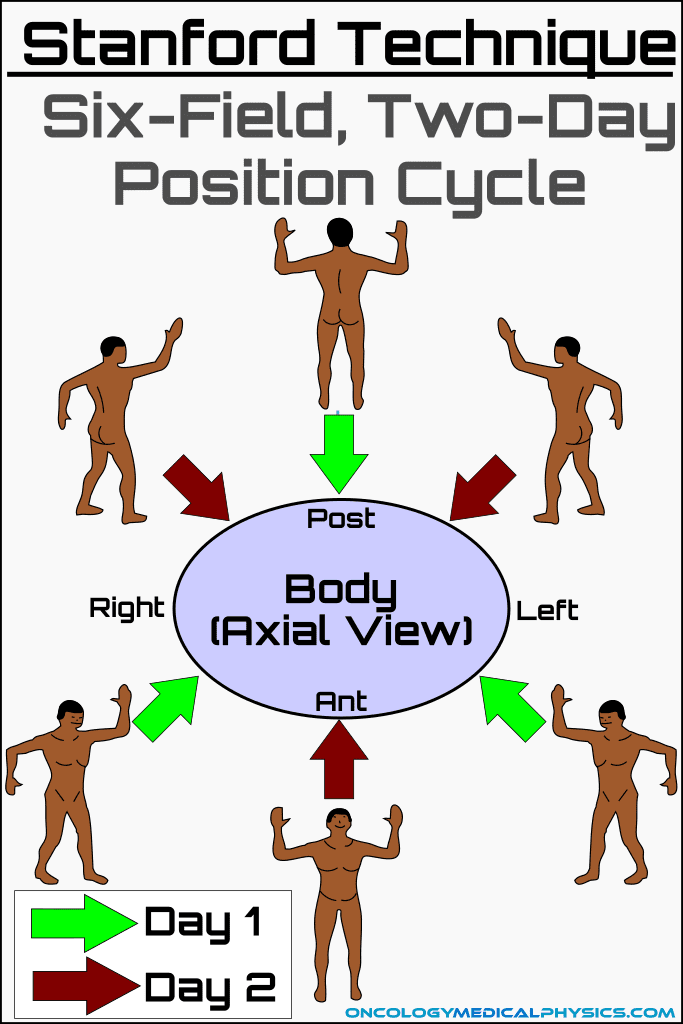
The Stanford technique utilizes 6 dual field patient positions which are delivered in sets of 3 fields on sequential days. Use of 6 positions improves uniformity over a 4 field technique and is less complex than an 8 field or continuous rotation technique.
Important Setup Points
- Patient is elevated off floor to reduce floor scatter dose.
- A scatterer is a Lucite (acrylic) panel about 1cm thick placed 20cm in front of the patient during treatment.
- The scatterer induces large angle scattering near the patient which improves dose uniformity but also reduces penetration and leads to less steep dose fall off.
Use of Boosts
- Boost are used to cover areas underdosed by the TSET delivery. Such areas include:
- Inframammary region
- Perianal region
- Inner buttocks and thighs
- Perineum
- Thick cutaneous tumors may also require a boost due to their depth.
- Boost may be delivered by electron or orthovoltage (~120kV) photon fields.
- Boost fields should assure a surface dose of at least 50% of prescription dose.
- Boosts improve progression-free survival by approximately 10-20%.
Patient Shielding
- Areas to be shielded
- Eyes must be shielded to <15% of prescription dose at surface.
- To prevent back scatter from increasing eyelid dose, eye shields may be coated with paraffin.
- Fingers
- Tops of feet
- Eyes must be shielded to <15% of prescription dose at surface.
- A common shield thickness of lead for 4 MeV electrons is 2mm.
- Eye shields are likely to be thinner as they are placed under the eye lid.
Potential Adverse Effects
| Adverse Effect | Incidence Rate |
|---|---|
| Erythema | 100%1 |
| Complete temporary alopecia (hair loss) | 100%1 |
| Temporary Nail Statis | 100%1 |
| Edema of hands and feet | <50%1 |
| Anhidrosis (reduced ability to perspire), Parotiditis, and gynecomastia (in males) | <3% each1 |
| Chronic nail dystrophy, chronic xerosis, permanent alopecia | <1% each1 |
| Mortality due to TSET | 0%1 |
| Immunosupression is common making infection an important cause of marbidity and mortality2 | Common in advanced MF patients.2 |
1. Total skin electron radiation in the management of mycosis fungoides: Consensus of the European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project Group. J Am Acad Dermatol. 2002 Sep;47(3):364-70.
2. L. Gunderson L, E. Tepper J. Clinical Radiation Oncology. Elservier Health Sciences; 2007.
Alternatives to the Stanford Technique
Several alternative treatment methods exist including the 4 dual-field and 8 dual-field techniques. Continuous rotation, in which the patient is placed on a rotating platform, is also sometimes used. Pendulum Arc, in which the treatment head is continually rotated in a 50 degree arc, is sometimes used to avoid the match line inherent in all dual-field techniques.
TSET Dosimetry
Calibration point is positioned along the center of the treatment plane at the height of linac isocenter (sees figure above) at depth of maximum dose.
Calibration point dose is the dose measured at the calibration point for a single dual-field (i.e. two fields angled at approximately +20° and -20°).
Calibration point dose output factor (not defined in TG-30) is the calibration point dose per MU of each treatment beam in the dual field. Unit: cGy/MU. (E.g. If the superior and inferior field each deliver 100MU and the calibration point dose is measured as 4cGy, the calibration point dose output factor is 4cGy/100MU = 0.04cGy/MU.)
Treatment skin dose is defined as mean dose along a circle near the surface of a cylindrical polystyrene phantom 30cm in diameter and 30cm high which has been irradiated by all six dual fields.
B factor is a factor that relates the calibration point dose to the treatment skin dose. B factors are typically between 2.5 and 3.1 because the calibration point receives dose contribution from approximately 3 fields.
![]()
Monitor Unit Calculation
Monitor units for a TSET deliver may be calculated as in the below equation. The total MU delivered for all fields will be 6 times the MUsingle field.
![]()
Common TSET Dosimeters
- Parallel-Plate Ion Chambers
- Required by TG-30 and TG-51 for calibration of absorbed dose.
- Measurement of depth dose.
- Measures ionization which must be converted to dose.
- Diode detectors
- Provide good spatial resolution and do not require significant correction between ionization measurement and absorbed dose.
- Film
- Useful for measuring treatment skin dose across entire plane
- May be useful in depth dose
- Thermoluminescent dosimeters
- Useful for patient dose monitoring
Navigation
Not a Premium Member?
Sign up today to get access to hundreds of ABR style practice questions.