Stereotactic Radiosurgery
Selected Readings
AAPM TG-42: Stereotactic Radiosurgery (external link)
Overview
Stereotactic Radiosurgery, commonly referred to as SRS, delivers a tumoricidal dose to small targets in a small number of fractions. SRS typically refers to a single fraction cranial radiosurgery and may be distinguished from FSRT (fractionated stereotactic radiosurgery) which uses up to 5 fractions for cranial treatments.
SRS was first described in 1951 by a Swedish Neurosurgeon (Lars Leksell) using a stereotactic frame and a 0.2MeV x-ray therapy machine.
Unlike traditional fractionated radiotherapy, which relies partly normal tissue sublethal damage repair to spare normal tissues, SRS relies on tight margins and rapid dose fall off to prevent normal tissue complications.
Key Point: Stereotaxis has historically referred to the use of a 3D coordinate system to localize a target. With modern imaging, however, use of an external localization system is often considered unnecessary.
SRS Treatment Planning
Patient Selection
Treatment of up to 5 lesions is typical although as many as 10 lesions have been treated with SRS.
Target size is often limited to <4-5cm as unacceptable normal tissue dose volumes become difficult to avoid beyond this size.
Other factors such as the shape (circular is preferred) and target distribution (increased inter-target distance is preferred) must be considered when selecting SRS candidates.
Prescription and Prescription Isodose Line
Prescription for tumors and metastasis are usually limited by nearby tissue tolerances, often associated with the volume of normal tissue receiving 12Gy. As such, smaller tumors will receive a higher prescription dose than larger tumors.
Prescription isodose line refers to the dose level of the prescription. For example, a prescription may be written: 21Gy to the 80% isodose line. In this example, the maximum dose would be 21/0.8 = 26.25Gy.
- Prescription isodose line is chosen to achieve a given coverage level of the target (often >99%).
- For most 6MV single isocenter C-arm linac delivered SRS plans, the prescription isodose line will be around 80%.
- Small fields and plans using sphere packing (especially Gamma Knife) may have prescription isodose lines as low as 50%.
Key Point: Low prescription isodose lines are used to optimize normal tissue sparing by improving conformality. However, there is some evidence that the resulting hot spots increase intratarget radionecrosis which is an adverse effect.
Margin Size
Although a large number of studies have indicated the efficacy of a 0mm treatment margin (i.e. PTV = CTV) this decision should be made on a site-by-site and patient-by-patient basis.
Several factors influence choice of margin size including:
- Expected target and organ motion during treatment
- Mechanical factors influencing precision and accuracy
- Isocenter positioning
- Imaging
- Expected dose gradient at field edge
- Contouring uncertainty
- Human variability
- Voxel size, image registration, and resampling
General Planning Techniques
Because SRS techniques depend upon highly accurate and precise delivery of a conformal dose distribution, several planning strategies will be nearly universally applied.
Combined MRI/CT Imaging
Magnetic Resonance (MR) imaging is valued in treatment planning as it is able to produce superior soft tissue contrast to CT images. This is especially valuable in SRS planning were targets are of similar density to their surrounding tissue and have a small size.
CT imaging is used to generate the treatment plan because of its superior spatial linearity, high resolution, and direct correlation between CT number and tissue density.
A fusion of the MR and CT images provides the best of both worlds. After image registration, the fused MR of the fused image set is used to generate target contours. The CT, which is also associated with the contours, is then used to generate the treatment plan.
Non-coplanar beam arrangements
Non-coplanar beam arrangements refers to using multiple angles of beam incident which do not exist on the same plan. This technique improves the conformality of the dose distribution and reduces surface dose.
Large number of beam angles
The large number of beam angles additionally serves to improve conformality. For c-arm linear accelerators, arcs are likely to be used in which the beam is continuously on during gantry rotation at a given angle.
Rigid Immobilization
The highly conformal dose distribution presents significant potential for geometric miss if the target is not precisely localized. Historically, this has been achieved using a stereotactic head frame but real time surface tracking is reducing the need for this invasive approach. Today rigid masks are becoming more popular.
Optical Tracking
Optical tracking uses a camera system to precisely localize the patient in real time. Optical tracking may either track to location reflective markers placed on the patient or the directly track the surface of the patient. These systems are extremely valuable in both reducing risk of geometric miss and decreasing treatment time through reduced need for repeat x-ray imaging during setup.
Key Point: Prescription dose is often limited by normal tissue tolerance. As a result, smaller tumors will often have a higher prescription than larger tumors.
Immobilization: Frame Based vs Frameless SRS
Frame Based
An SRS frame refers to an immobilization and registration device physically attached, usually by pointed screws, to the patient's cranium.
Historically, frames included a radio-opaque fiducial marking system which allowed orthogonal port films to verify precise 3-dimentional alignment. This function has been largely superseded by the proliferation of high quality on-board cone-beam imaging.
Frame based SRS may be either couch mounted" or "floor stand mounted."
Note that although the screws will penetrate the patient's skin, they do no significantly penetrate the cranium and are generally well tolerated by patients.
Advantages
- Highest degree of immobilization
- Benefits from but does not require intra-treatment position monitoring
Disadvantages
- Requires neurosurgeon to place frame
- Requires same day placement, simulation, planning, quality assurance, and delivery
Frameless
Frameless SRS uses an external mask in conjunction with intra-fraction position monitoring to achieve precision.
Initial target alignment is achieved through cone-beam CT (CBCT) imaging. Primary alignment typically focuses on fixed bony anatomy with fine-tuning based on nearby soft tissue.
Intra-fraction position often achieved using an optical camera to monitor patient surface or externally located fiducial markers.
Gating or real time tracking may be used to assure geometric accuracy of treatment delivery.
Gating shuts off the treatment beam when the target is found to be outside of its designated region.
Tracking causes the beam to follow the target as it moves.
Advantages
- Allows simulation, planning, and delivery to take place on different days
- Less invasive to the patient
Disadvantages
- Inherently less immobilizing than frame based deliveries
- Real-time positioning system requires additional physics quality assurance
Planning Techniques
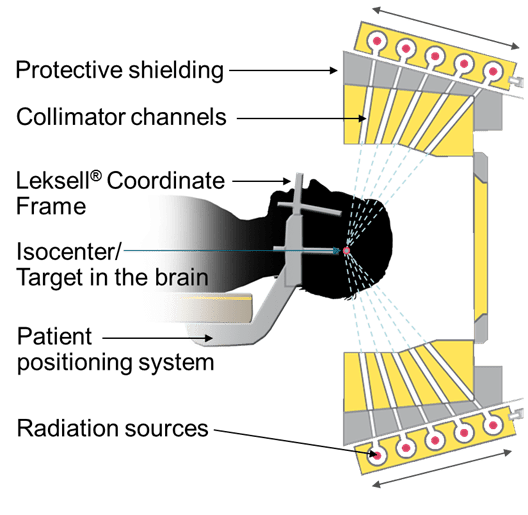
Fixed Collimator Sphere Packing
Fixed circular collimation, as achieved in Gamma Knife and cone base deliveries, produces a roughly spherical dose distribution. Because many tumors are not spherically shaped, a technique known as sphere packing is used.
Sphere packing fills the target volume with multiple spherical dose distributions of varying sizes to achieve a conformal net dose distribution.
The sphere packing technique is usually achieved by first filling in the largest area with a large dose sphere and proceeding to fill in the remaining area with smaller and smaller spheres.
Advantages
Cone based plans achieve the sharpest dose fall off and therefore have the greatest geometric window.
Disadvantages
Large irregular volumes often have significant dose heterogeneity within the target.
Complex targets require multiple cone sizes and isocenters. This greatly increased treatment time.
MLC Based Conformal Arc
Conformal arc planning uses an MLC which changes shape to conform to the shape of a target during a delivery arc. Because the MLC can produce larger and more irregular fields than a cone, MLC based plans typically use less isocenters and thereby require less treatment time.
Advantages
Single isocenter per target
For multiple closely packed targets, a single isocenter may be sufficient.
Simplifies treatment planning
Shortens delivery
Often achieves lower hot spots for irregular targets
Disadvantages
Larger penumbra than cone because final collimation is farther from target.
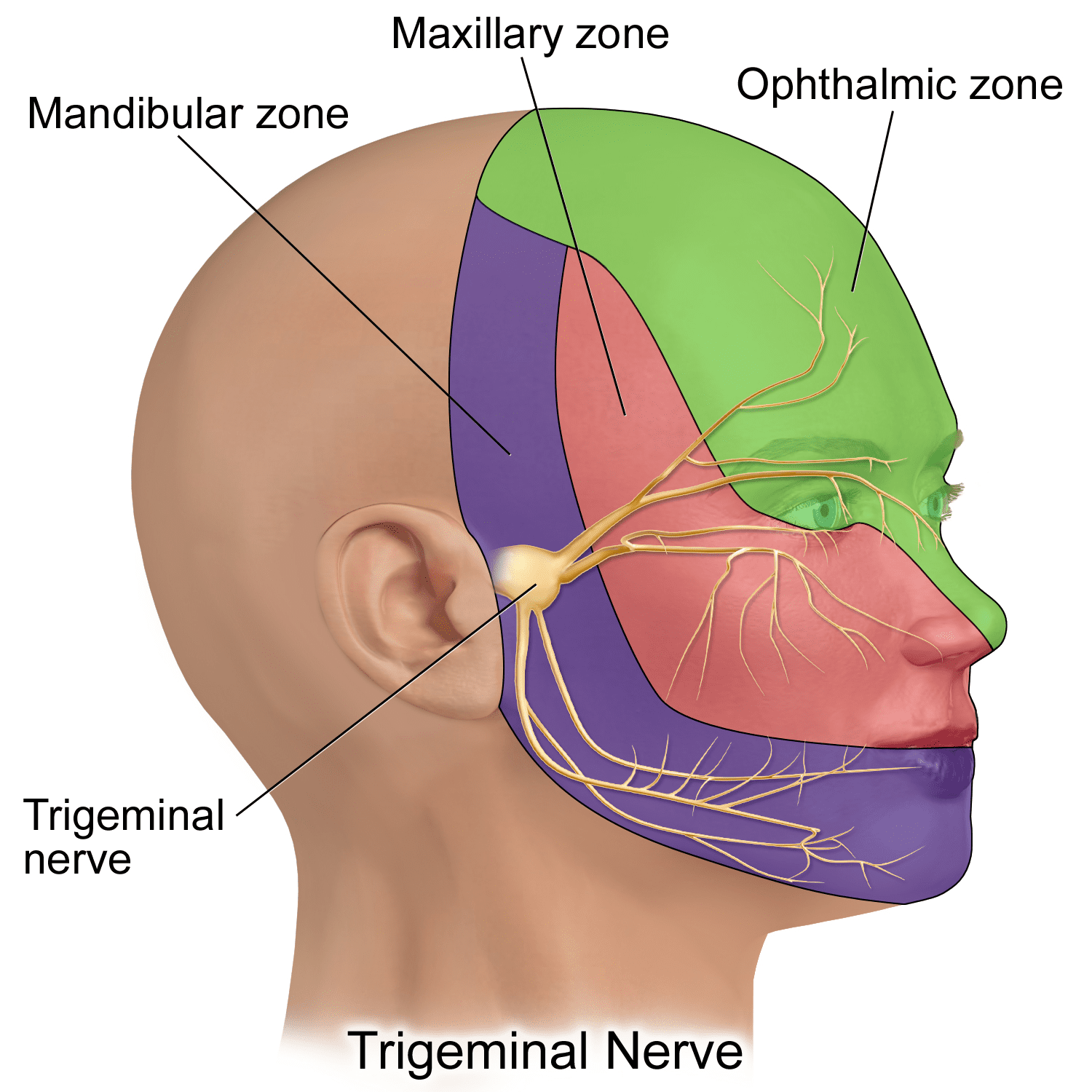
Choosing an MLC or cone: Choice of cone or MLC based planning involves several trade-offs. Cones are most commonly used for small, spherical targets or those which require the sharpest possible dose fall-off such as Trigeminal Neuralgia. Dynamic MLCs are favorable for their ability to treat large or irregular targets and to do so significantly faster than cones.
Treatment Sites
Intracranial Tumors
Primary Cancers/Surgical Cavity
Background: SRS has been used in the management of most intracranial tumors. However, malignant tumors may be poorly suited for SRS because of their high alpha/beta ratios and probability of proliferation. The most common cancers for SRS treatment are benign meningiomas and malignant gliomas.
Common Prescriptions:
Benign Meningiomas: 12-20Gy
Target: MRI enhancing boarder of lesion plus optional PTV margin of about 1mm.
Outcomes: Outcomes vary significantly with disease.
Benign meningiomas experience excellent control (>97% at 5 years) with SRS.
Glioblastoma Multiforme, the most common glioma, experience generally low rates of control.
Metastases
Background: SRS for brain metastases is an alternative to surgical removal or whole brain irradiation. These metastasis are often from a lung primary tumor.
Common Prescriptions: 12-21Gy
Target: PTV = CTV + (0 to 2mm margin)
Outcomes: Control of metastatic brain tumors, especially those less than 2cm in diameter, is good and comparable to surgical removal. Clinical trials indicate SRS with 3-4 lesions may improve survival and reduce normal tissue toxicity (i.e. memory loss) as compared with whole brain irradiation. Treatment of 5 or more metastases using SRS does not appear to convey a survival advantage over whole brain irradiation but may reduce cognitive losses and allows for future salvage therapy.
Alternative Treatments:
Surgical Resection - May be appropriate for a small number of superficial metastases.
Whole Brain Irradiation - May be appropriate for large lesions or a large number of metastases (>4).
Functional Disorders
Trigeminal Neuralgia
Background: The first SRS treatments administered were for sufferers of trigeminal neuralgia. Trigeminal neuralgia is a disorder characterize by severe, stabbing, facial pain. The disorder is, in most cases, thought to be caused by compression of the trigeminal nerve root. SRS is a second line treatment used for cases resistant to drug treatments.
Common Prescriptions: 50-90Gy; 85Gy (most common)
Target: SRS for trigeminal neuralgia targets a small segment of the trigeminal nerve between the brainstem and Meckel's cave.
A 4mm cone size is often selected.
Outcomes: Pain relief is achieved in approximately 90% of patients with the mean time to relief of about 24 days. The most common toxicity is facial numbness.
Arteriovenous Malformation
Background: Atriovenous Malformation (AVM) is an abnormal tangle of blood vessels connecting veins and arteries in the brain. The exact cause of AVM formation is not clear but most AVMs are congenital (present at birth) and are not generally hereditary.
Atriovenous malformation may present as headaches, seizures, or other neurological symptoms associated with hemorrhage. Most AVM SRS treatments are used to prevent repeat bleeding after an initial hemorrhage.
Diagnosis: AVM is diagnosed using CT, MRI, or Cerebral Arteriography.
Cerebral Arteriography (Angiography) involved inserting a catheter into the femoral artery and guiding it to the brain using fluorography. Once in the suspected region, contrast is injected allowing for detailed images of the local vessels.
Common Prescriptions: 16-25Gy
Outcomes: Obliteration of the AVM takes place over 1-3 years following SRS with an ultimate success rate of 54-92%. Potential tissue toxicities include seizure, headache, neurological deficit, necrosis. Reducing the 12Gy volume outside of target can reduce toxicity.
Alternative Treatment Options:
Surgical Resection - Common in superficial and other easily accessed AVM locations.
Enovascular embolization - A glue-like substance is injected into the AVM preventing blood flow.
SRS Specific Treatment Machines
Today SRS is commonly delivered using a standard or modified C-arm linear accelerator. Several specialized machines exist for this purpose however, each having its own advantages.
Gamma Knife
The Gamma knife was first created by the originator of SRS, Neurosurgeon Lars Leksell, and a physicist, Borje Larsson in the late 1960s. Today Gamma Knife is owned by Elekta and several similar products are made by other manufacturers (GammaART by Cancer Care International, GyroKnife by GammaStar).
Cyber Knife
The CyberKnife system is a linac based SRS delivery system mounted on a robotic arm.
Key Features
X-band linac mounted on robotic arm
Collimation provided by fixed cone or a variable MLC-type collimator.
Targeting Precision 1mm
Navigation
Not a Premium Member?
Sign up today to get access to hundreds of ABR style practice questions.